Abhishek Prasad, Ph.D., associate professor of biomedical engineering, was awarded a $2.79 million five-year grant to study the impact of iron accumulation from microelectrodes on the brain, while Patrick D. Ganzer, Ph.D., assistant professor of biomedical engineering, received a $2.43 million grant to see if pairing muscle movements with nerve stimulation can improve function following spinal cord injury.
“These NIH grant awards show the significance of the College of Engineering’s collaborative initiative with the Miller School of Medicine that brings neural engineering and biological science together to address highly challenging medical conditions,” said Fabrice Manns, Ph.D., professor and chair, Department of Biomedical Engineering. “We greatly appreciate the support from The Miami Project to Cure Paralysis and our shared research space in the Lois Pope Life Center on the medical campus. We believe these grants are just the beginning for our dynamic multidisciplinary research.”
Neural Engineering Institute Co-directors W. Dalton Dietrich, Ph.D, and Suhrud Rajguru PhD also emphasized the importance of Prasad and Ganzer’s neural engineering studies. “Our multidisciplinary approach holds great promise for addressing current needs in improving function in people living with brain and spinal cord disorders. These major research grants are a testament to our outstanding faculty and the collaborations in research and education that the Institute for Neural Engineering has spurred between the Medical School and College of Engineering.”
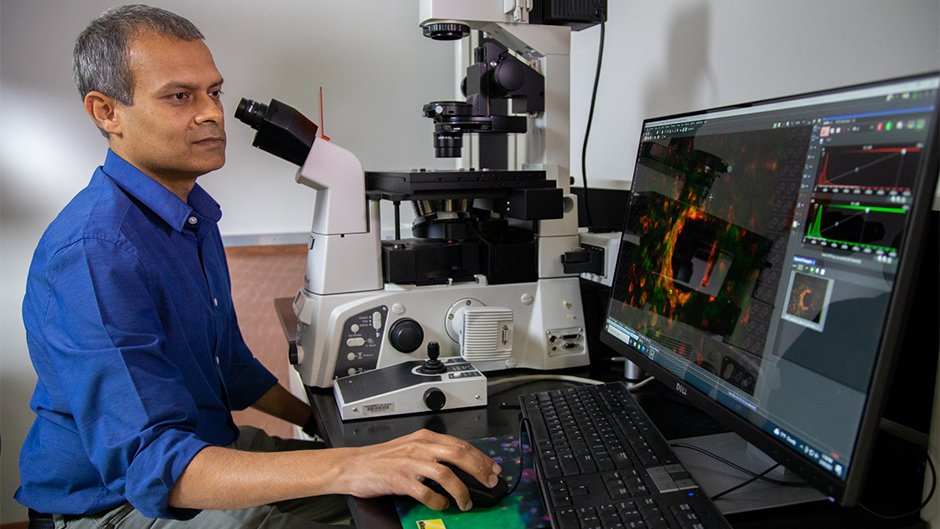
Microelectrode implants
Microelectrodes implanted in the nervous system are critical tools for research and in clinical applications that use neuromodulation to treat neurological disorders. In a brain computer interface (BCI), microelectrodes are used to record brain activity that have been shown to restore function to people living with paralysis via control of external devices such as computer cursors, robotic arms, or one’s own limbs through functional electrode stimulation. Alternately, in a deep brain stimulation (DBS) application, current can be passed through microelectrodes to the nervous system tissue to treat patients with multiple neurological disorders. However, the electrodes gradually degrade and tend to fail over time. “Bleeding occurs when the electrodes are surgically implanted,” said Prasad. “This leads to entry of hemoglobin into the brain tissue resulting in the release of free iron in the tissue.” Prasad hypothesizes that the accumulation of iron at the site of electrode injury contributes towards overall neuroinflammation and oxidative stress. Further, the proposed studies will study the effects of iron chelation on neuroinflammation, oxidative stress, and the electrode function, at the electrode-tissue interface surrounding brain tissues.
As principal investigator of the NIH grant, “Effects of Iron Accumulation in Intracortical Implants and Protection by Iron Chelation,” Prasad is studying the effect of iron accumulation and its chelation in intracortical microelectrode implants. In collaboration with Dr. Jean-Hubert Olivier, Ph.D., associate professor of chemistry, the team will develop materials that will enable local release of iron chelators at the site of injury in an effort to mitigate the neuroinflammatory response and improve long-term function of microelectrodes.
"I would like to thank the University of Miami Clinical and Translational Science Institute (CTSI) for providing the pilot funding through their Pilot Research Award during the last year," Prasad said, "which enabled us to continue doing the work and gather important preliminary data for the proposal. Without this support, we could not have carried out the preliminary work, and I am grateful for the CTSI’s support."
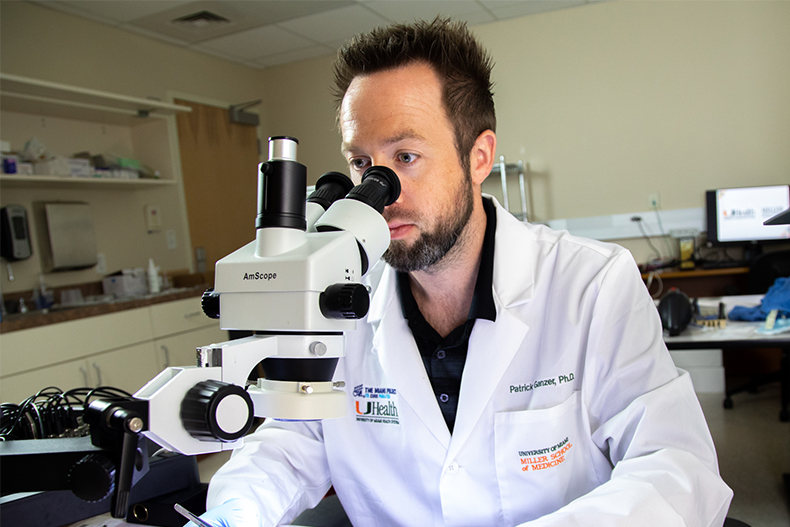
Spinal cord therapy
Precisely timed vagus nerve stimulation (VNS) paired with muscle movements could improve the rehabilitation of patients with severe cervical spinal cord injuries, according to Ganzer, who is the principal investigator for the NIH-funded study, “Enhancing Sympathetic Outflow Control Following Spinal Cord Injury Using Targeted Plasticity Therapy.” Ganzer is collaborating with Dr. Mark Nash (Associate Scientific Director, The Miami Project to Cure Paralysis; Professor of Neurological Surgery & Physical Medicine and Rehabilitation), Dr. Pantelis Tsoulfas (Associate Professor of Neurological Surgery, University of Miami), and Dr. Robert Hamlin (QTest Laboratories) on the awarded work.
The primary goal of the preclinical study is to improve neural signaling to the upper limbs and the cardiovascular system. “In many patients with spinal cord injuries, control of the heart and blood vessels becomes weaker,” he said. “As a result, patients may find difficultly being positioned upright and feel muscle fatigue more quickly during their physical therapy sessions.”
Ganzer said his studies have shown that repeatedly pairing brief bursts of VNS with movements during rehabilitation significantly improves upper limb motor function. “Now, we want to expand on that work, and open up new therapeutic strategies for cervical spinal cord injuries.”