A few months ago, as the coronavirus pandemic began to permeate the United States, Dr. Carl Schulman, executive dean for research and professor of surgery at the Miller School of Medicine, could not help but notice the shortage of protective equipment for health care professionals distressing the nation. In particular, he worried about the lack of N95 masks, which filter out 95 percent of airborne particles, making them the top choice for many health care workers eager to protect themselves from COVID-19.
“When the first mini peak of COVID-19 happened, people just couldn’t get these N95 masks,” said Schulman, who often wears the typical disposable masks as a physician in the burn unit and trauma intensive care unit at Jackson Memorial Hospital.
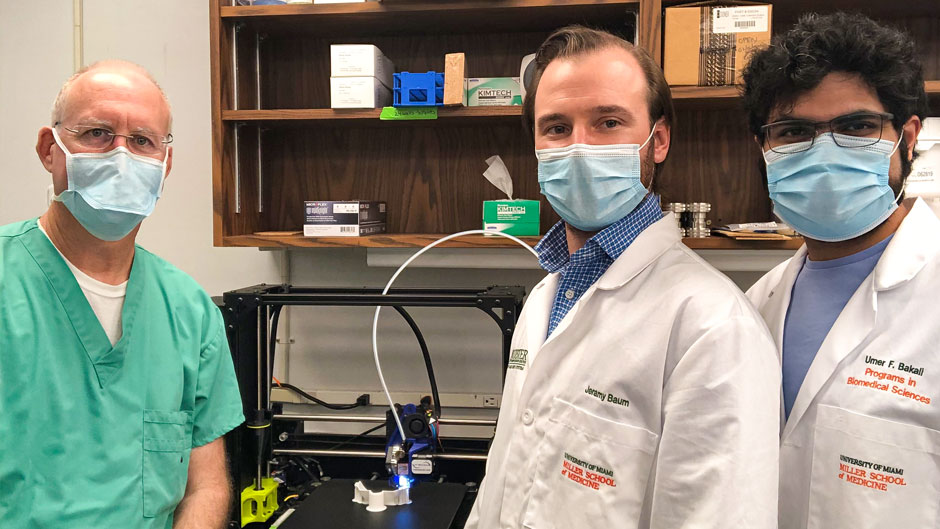
Schulman, who grew up building things with his father, a contractor, recalled that his lab had recently purchased a 3D printer for another project. He saw an opportunity to use the new equipment to design a washable, reusable N95 mask.
“We are trying to recreate these masks in a way that anyone could reproduce and use them,” he said, acknowledging that elastomeric masks similar to these already exist but are expensive and in short supply. “If we can get it finalized, this would be helpful not only locally but nationally and globally.”
With his collaborators, Sylvia Daunert and Sapna Deo, professors of biochemistry and molecular biology, as well as graduate student Umer Bakali and recent Ph.D. graduate Jeramy Baum, Schulman’s team got to work in late March, melding designs he found online and printing them to test for comfort, durability, and facial fit. Ramon Montero, biomedical engineering assistant professor of professional practice, and Max Jarosz, a model shop manager in the School of Architecture, also consulted and assisted with the team on their own design as part of the University’s COVID-19 Preparedness Committee. Soon, Schulman’s efforts to buy materials and refine the mask design were buoyed by funding from a Rapid Response Grant awarded by the University’s Office of the Vice Provost for Research.
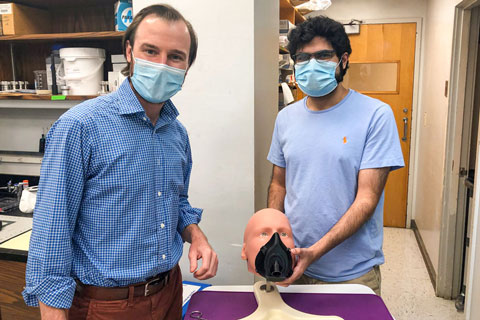
After three months of trial and error, Schulman said the team is very close to a prototype. The mask features a hole in the middle, where different types of medical pathogen filters can be inserted (and replaced) to purify air circulating through the mask to protect the wearer and surrounding people. These filters are readily available in most hospitals because they are used for respirators and ventilators, Schulman said. The next step: securing a good, comfortable seal so the masks will be airtight.
“We’re down to the last bit, the seal, which has been the most challenging part,” he said.
Baum and Bakali have spent the past month working on the mask seal, which they hope will enhance the comfort of health care personnel who have been wearing the disposable N95 masks past their recommended duration.
“A solution like this could help decrease the discomfort for medical personnel who are wearing these one-time-use N95 masks long-term,” Baum said, “Because right now, they are getting rashes and lesions, and some are even getting scabs from wearing these masks for so long.”

Also, because their masks can be disinfected, if used widely they could help cut down on biomedical waste, which has ballooned since the pandemic began, Baum added.
“These masks could decrease the environmental impact of personal protective equipment because the impact right now in the world is huge,” he said.
After they are satisfied with the seal, Schulman’s team will test the masks to confirm they are able to meet the N95 standards. Once all the imperfections are ironed out, the team plans to write a paper about the process and make their design available to anyone who wants to create their own 3D-printed N95 mask.
“I see the benefit of this project not just in the U.S. but in the less developed world as well,” Schulman said, noting that all is needed is a standard 3D printer and basic materials. “Instead of needing 1,000 masks for 10 days, you could print 100 of these, and they could last indefinitely.”