At the onset of the COVID-19 pandemic in early 2020, individuals with no medical insurance and employees experiencing furloughs or layoffs as lockdowns took hold grappled with the possibility of facing the need for medical treatment for the novel coronavirus without insurance coverage. Trump Administration officials at the Health Resources and Services Administration (HRSA), a division of the Department of Health and Human Services, had to quickly determine a path forward to enable access to treatment for people in the extraneous circumstance. The officials opted to create the Provider Relief Fund, a reimbursement program in which the federal government provided payment at Medicare rates to health care providers for each uninsured claim. The program prohibited providers from passing on any costs to patients, allowing the uninsured to receive full coverage for all treatment related to a COVID-19 infection.
Early critics of the policy contended that the PRF did not allow for enough clarity since some conditions such as pneumonia or kidney failure could not always be traced to a COVID infection as opposed to other health causes. Democrats called for an additional open enrollment period so that people without insurance could enroll under the Affordable Care Act. A second option entailed implementing a nationwide emergency expansion of Medicaid.
But these options signified too broad a scope beyond the priority of ensuring coverage strictly for COVID-related treatments, explains Miami Herbert Business School’s Karoline Mortensen, professor of health management and associate dean of business programs.
“Rather than a more comprehensive, full access to health insurance, the PRF was guaranteeing providers that they would get paid for treating the uninsured patients,” she says. “It was a more limited version of coverage with a targeted focus on COVID-19.”
To study the efficacy of the program, Mortensen partnered with Stephen T. Parente, who served as senior economist and chief economist for health policy on the Council of Economic Advisers for former President Donald Trump and formed part of the team tasked with making the quick determinations regarding the PRF, which included establishing the program as a public-private partnership. Disbursements occurred through a private insurer with access to the bank accounts of the vast majority of providers rather than through a government entity that would have had to create new payment mechanisms.
Mortensen and Parente, today a professor and the chair of health finance at the University of Minnesota’s Carlson School of Management, set out to analyze how efficiently funds under the program had been distributed among states from April 2020 to Sept. 2021 for individuals between the ages of 19 to 64. Specifically, did states get reimbursed adequately according to their percentage of the uninsured population?
“We were interested in learning if the program was having the very targeted response that it was meant to have,” Mortensen says.
Their study, recently published in the JAMA Health Forum journal, consisted of a cross-sectional comparison of state reimbursement rates for the uninsured to each state’s percentage of the relevant population. The authors used readily available claims and distribution data by the HRSA and the Centers for Disease Control and Prevention. To account for coverage through state-level Affordable Care Act Medicaid expansion, the authors classified states as either a Medicaid expansion or non-Medicaid expansion state.
Mortensen and Parente found that states with the largest uninsured populations, such as Texas, California, and Florida, were among those with the highest reimbursement levels, as shown in the graph below. Also, Medicaid expansion states generally used less than their proportionate share of the program distribution, though New Jersey, Maryland, and Nevada took in greater shares.
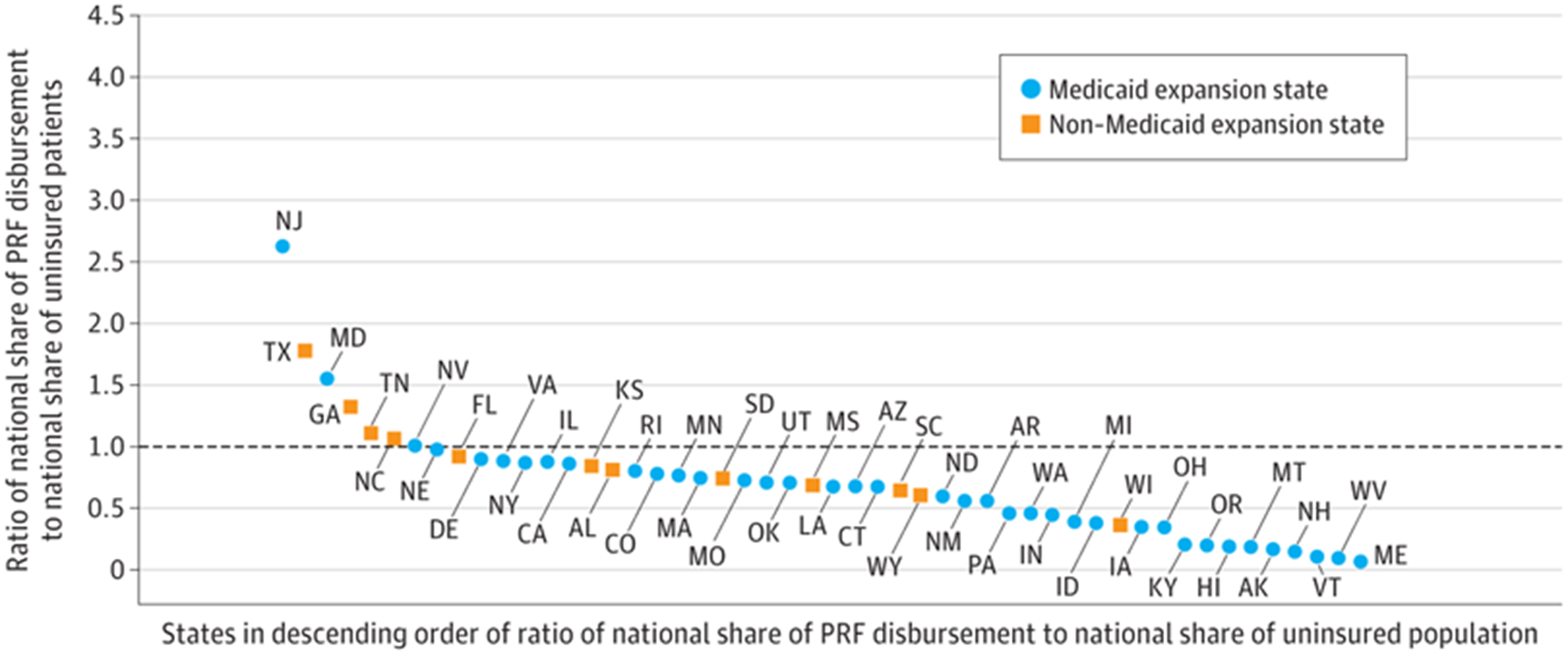
The findings show that states with the greatest population demands received the larger share of funds, suggesting that the PRF program successfully enabled the disbursement of funds to the providers who needed them most as they cared for a greater bulk of the uninsured population.
As the authors state in the study: “As a policy mechanism to address the largest national health crisis in generations, the program served rough justice (a set of quick and decisive actions by the HHS leadership without prior policy precedent in a time of national crisis) to states with some of the highest shares of the uninsured population.”
The analysis additionally reveals that state Medicaid expansion programs protected the vulnerable population by giving them access to insurance and hence requiring less than a state’s proportionate share of the PRF funds, serving as another effective strategy. Mortensen highlights, however, that further investigation may help explain the wide variation in reimbursement levels among the Medicaid expansion states. The study may also open avenues to evaluate programs similar to the PRF for testing and vaccination of the uninsured.

