The United Nations' goal of ending AIDS around the world by 2030 is undeniably ambitious, but within tantalizing reach. Thanks to medications that suppress the once-fatal human immunodeficiency virus and prevent its transmission, new infections have dropped by nearly 50 percent over the past two decades.
Yet in 2017, Miami held the dubious distinction of being No. 1 in the nation for new HIV cases, with a rate nearly four times the national average.
Why is not a big mystery to behavioral and social scientists at the University of Miami, who were recently awarded a four-year $3.32 million grant by the National Institute of Mental Health to establish a developmental AIDS Research Center to promote research aimed at curbing the local epidemic.
As Steven Safren, principal investigator on the grant and director of the new Center for HIV and Research in Mental Health, or CHARM, notes, controlling Greater Miami’s HIV/AIDS epidemic will not happen without addressing the mental and minority health disparities that help perpetuate the disease today—disparities that most affect the poor and marginalized, and the racial, sexual, gender, and ethnic minorities who live in view of the area’s gleaming new condos and sun-splashed beaches.
“HIV is different today than it was when it first started, largely among gay men,” said Safren, a professor of psychology who also heads CHARM’s administrative core. “Although men who have sex with men still comprise the majority of individuals living with HIV, it is now largely a disease of big-city poor and intertwined with behavioral health issues, like depression, problematic substance abuse, traumatic stress, stigmas, discrimination—all the things that make it very hard for a lot of people to access treatment, to stay in treatment, and to get the best benefit from treatment.”
Under ideal circumstances, every person infected with HIV would be promptly diagnosed and immediately start taking the antiretroviral therapy (ART) that would reduce their viral load to an undetectable level. That would not only keep them healthy, but would eliminate their risk of passing on the disease, either through sexual contact or sharing used needles, that has killed more than 34 million people around the world since the first U.S. cases were diagnosed in 1981.
But adhering to a daily drug regimen often isn’t a priority or even possible for people living with HIV who worry about their next meal or a place to sleep, who have no way to get to the lone pharmacy that provides free medications, who battle unrelenting depression or struggle with substance use, who are traumatized by violence or sexual abuse, or who are cast aside because they are gay, transgender, dark-skinned, or from another culture and speak another language.
“When effective medication was discovered for HIV, the assumption was, OK, people are going to get it and take it, and we’re going to be done,” said Sannisha Dale, assistant professor of psychology and CHARM’s scientific director for community engagement. “But there was no attention being paid to the mental and psychosocial factors that would impact people gaining access to treatment, getting their meds, and staying on them. And we scientists didn’t do a very good job of engaging with the community experts on the ground.”
Though administered through the College of Arts and Sciences, CHARM is a cross-campus collaboration, encompassing faculty from multiple schools and complementing the Miller School of Medicine’s Center for AIDS Research (CFAR), which the National Institute of Allergy and Infectious Diseases first funded as a developmental center in 2007. Transitioning to a full-fledged center in 2012, the CFAR has been refunded through 2022, and focuses primarily on biomedical research aimed at ending HIV/AIDS.
Safren, who joined UM in 2015 after founding and leading the behavioral and social sciences core at Harvard University’s CFAR, and his CHARM co-directors, the Miller School’s Daniel Feaster, professor in the Department of Public Health Sciences, and Deborah Jones Weiss, professor of psychiatry and behavioral sciences, hope CHARM will follow suit. By creating a research infrastructure that will not only help curb Miami’s epidemic but be applicable to other under-resourced settings coping with uncontrolled epidemics, they believe CHARM will earn full-fledged center status after its four-year developmental period.
Although CHARM is the NIMH’s seventh AIDS Research Center, it is the first in the South, the U.S. region hardest hit by HIV/AIDS. Like Miami, the South has many pockets that lack sufficient resources or face significant barriers to fight the epidemic with the existing tools that could, in theory, eliminate AIDS by 2030. That’s the goal the Joint United Nations Programme on HIV/AIDS adopted in 2014, and that President Donald Trump embraced in his last State of the Union address.
As it stands today, Miami in particular, and South Florida in general, will not meet even the U.N.’s interim goal for 2020. Known as the 90-90-90 goal, it calls for 90 percent of all people living with HIV to know their status; 90 percent of those who know their status to be on ART; and 90 percent of those on ART to have suppressed viral loads, making their disease noncommunicable.
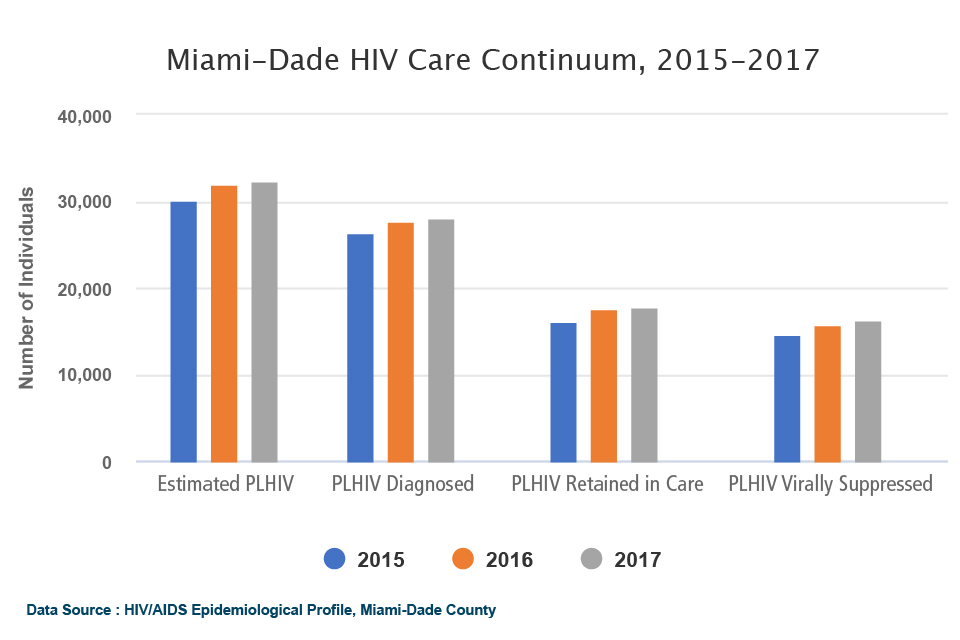
As of 2017, of the 87 percent of the people living with HIV (noted as PLHIV in the chart below) in Miami-Dade County who knew their diagnosis, only 64 percent of them were on treatment, and only 58 percent of them were virally suppressed. Yet, as Safren noted, “the Miami-Dade County Health Department has far fewer resources dedicated specifically to HIV/AIDS prevention and treatment than health departments in cities like Boston, New York, and San Francisco, which have seen significant reductions in their rates of new HIV infections.”
 The lack of such resources are among the structural barriers that, by working with state and community partners, CHARM investigators hope to resolve. They’re also gearing up to support and catalyze the high-impact research needed to develop prevention and care programs for the most challenging and vulnerable populations. In addition to the administrative core, which will be the hub for community engagement activities that are central to the center’s mission, CHARM has three other cores: a developmental core, and two unique research cores.
The lack of such resources are among the structural barriers that, by working with state and community partners, CHARM investigators hope to resolve. They’re also gearing up to support and catalyze the high-impact research needed to develop prevention and care programs for the most challenging and vulnerable populations. In addition to the administrative core, which will be the hub for community engagement activities that are central to the center’s mission, CHARM has three other cores: a developmental core, and two unique research cores.
The Developmental Core, which will award funding for pilot studies to early-career investigators, is designed to support and mentor UM’s growing cadre of behavioral health-related HIV/AIDS researchers. Led by Adam Carrico, associate professor of public health sciences and psychology who has conducted significant research on people living with HIV and substance use disorders, and the Department of Medicine’s Allan Rodriguez and Maria Alcaide, the core aims to award at least two grants a year to UM investigators engaging in research with community collaborations.
The Methods Core, led by Feaster, who has more than 30 years’ experience as a biobehaviorial statistician, and the Department of Public Health Sciences’ Raymond Balise, will help researchers design, implement, and analyze their studies.
Led by Jones Weiss and the School of Nursing and Health Studies’ Victoria Mitrani, the Mental Health Disparities Core will train researchers to pursue the kind of culturally competent, theory-driven approaches, tools, and interventions that address the mental health disparities among the diverse populations living with or at risk of contracting HIV/AIDS in South Florida.
“The fact is one size does not fit all,” said Jones Weiss, who has been conducting AIDS-related research around the world for more than three decades. “We have to be sensitive, knowledgeable, and respectful of racial and ethnic perspectives. Otherwise we will not connect to the people we want to help. But if we’re successful, we can put ourselves out of this job and that would be a true success.”
For information on CHARM, contact Paco Castellón, director of research support, at pcastellon@med.miami.edu or 305-243-0987.

