Imagine a heart beating outside of the human body. Imagine that the organ acts just like the real thing but can be handled and studied like any other object. What possibilities would that create for physicians, scientists, pharmaceutical researchers, and other scholars?
Imagine a heart beating outside of the human body. Imagine that the organ acts just like the real thing but can be handled and studied like any other object. What possibilities would that create for physicians, scientists, pharmaceutical researchers, and other scholars?
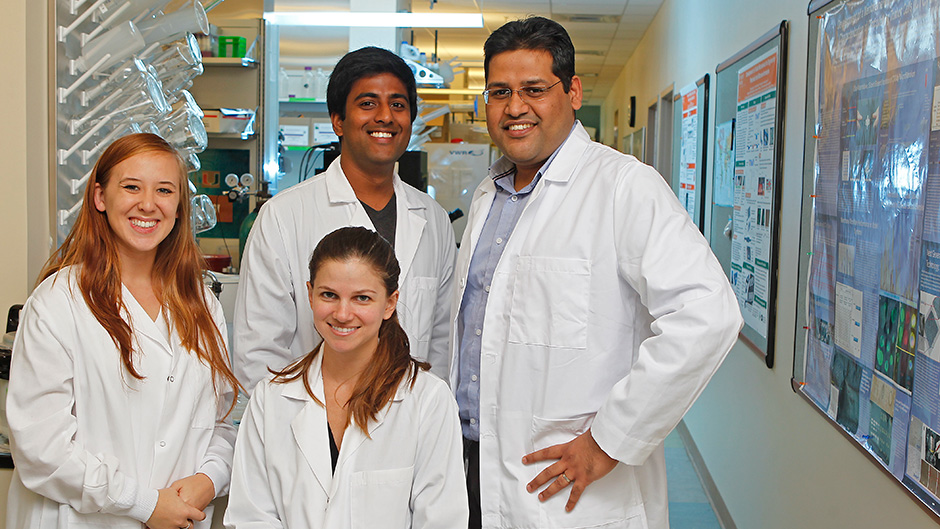
Ashutosh Agarwal, assistant professor in the departments of Biomedical Engineering and Pathology at the University of Miami, is ready to answer those questions. He is creating “Human Organs on Chips."
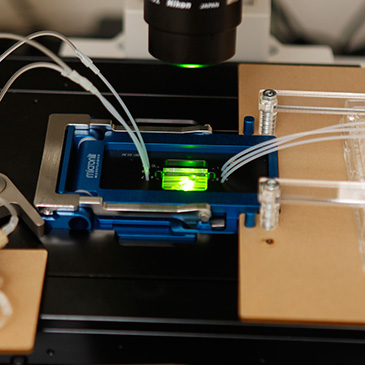
In a revolutionary new approach, he combines traditional engineering structures such as metal or plastic with stem cells from rodents and humans to create a heart, pancreas, and lungs that mimic the real organ – including normal functions and diseased organs. The chips, about the size of a USB stick or credit card, are created through 3-D printing and 3-D milling with intricate, precise measurements.
UM News spoke to Agarwal about his research. Here are some of his observations:
What excites you about this research?
Recreating human organ-level complexity in a dish, in both health and in disease, opens up several important applications. We can now test drug molecules before running clinical trials, dive deep into disease mechanisms, and create better stem cells for therapy.
What is the most important aspect of this approach?
Nobel Prize winning American physicist and visionary Richard Feynman famously said: "What I cannot create, I do not understand.” By building models of human disease on a dish, we will enhance the understanding of the underlying disease pathways. Current projects include type 1 diabetes, stage IV lung cancer, cardiac diseases, and idiopathic pulmonary fibrosis.
What kind of response has there been to your research in the past?
The significance of this research endeavor has been well recognized by federal funding agencies such as NIH, regulatory agencies such as the FDA, and received recent interest from pharmaceutical companies. The lab has received major grant funding from NIH. I have served on "Placenta on a Chip" workshop organized by Eunice Kennedy Shriver National Institute of Child Health and Human Development, "Wait What" conference organized by DARPA, as well as give a lecture at the "Futures of Cardiovascular Medicine" symposium by the American College of Cardiology (a primarily clinical conference).
Describe the process from being an idea to practicality.
We follow the engineering iterative process of Design --> Build --> Test.
Once we get interested in a disease model (typically through a clinical collaboration/announcement of a new funding initiative), we start with a physiology textbook. We study the template of how the body builds that organ and use that as a design template for our efforts in the lab.
In addition to mimicking the organ level structure, our devices allow evaluation of organ level function. We then populate these devices with cellular material sourced from human patients or stem cells. Based on the behavior of engineered tissues, we modify and optimize our devices. The last crucial step is validation by comparing our lab discoveries with clinical outputs.
Why is research in this area important (or relevant) for the average person?
Our tools will enable cheaper and faster drug development, discovery of therapies for some of the most intractable human diseases (such as type 1 diabetes, heart failure, lung cancer, and pulmonary fibrosis), and help make stem cell therapy a reality. Right now drug testing is first done on animals before it is approved for use on humans. That process is not always successful, and it is very expensive. We think we can make animal testing irrelevant.
What happens next?
The tools we are building in the lab need validation from two sources: clinicians, who are trying to understand and cure diseases, and pharmaceutical companies, who are developing new drugs. Validation from these two final 'customers' is the next step.
What's the coolest thing about this development or something unexpected about it?
The interdisciplinary nature of the work. Currently, I am managing a group of folks with very different backgrounds and expertise. My postdoc has a Ph.D. in space propulsion; one of my technicians has a medical degree, and the other is a stem cell expert.
My masters' student is a chemical engineer with expertise in fluid transport physics. The three Ph.D. students are working on creating a Heart on a Chip, Diabetes on a Chip and Pulmonary Fibrosis on a Chip. It's a rich collaborative environment and we learn from each other all the time!
The research is supported by the following: UM College of Engineering, Dr. John T Macdonald Foundation Biomedical Nanotechnology Institute at UM (BioNIUM; National Institutes of Health (Diabetes on a Chip); BioNIUM Research Award (Lung Cancer on a Chip), and UM-FIU Nanotechnology Award (Heart on a Chip).