Using data from room sensors and wearable devices that tracked the movement of preschool students and teachers, a team of University of Miami researchers simulated the spread of COVID-19 in school and found that reducing class size by half led to a significant drop in overall infections.
Add vaccinated teachers to the equation, and infections dropped without a reduction in the number of children. Even more noteworthy, in more than half of the simulations where both the classroom was at half capacity and the teachers were vaccinated, the first symptomatic infection never led to a second one.
“That’s exactly what you want,” said Daniel S. Messinger, professor of psychology and co-author of the study the team is sharing with Miami-Dade County Public Schools just after students resumed in-class learning under a mandate to wear masks.
“You don’t want a second symptomatic individual,” Messinger continued. “That’s when you win. When the teacher is vaccinated, when there are fewer kids in the class, there are fewer susceptible people. So, when somebody goes to school with COVID-19, our simulations showed that more than half the time, you’ll never get another symptomatic case.”
For the study, Messinger and co-authors from four departments capitalized on the rich, granular, and real-time automated observations that he and Lynn K. Perry, associate professor of psychology, began collecting in 2018 to understand the social interactions of preschoolers. In those previous studies, 11 teachers and 50 children between the ages of 2 and 5 wore small tags that emitted radio frequency signals as they went about their school day in four Miami-Dade classrooms.
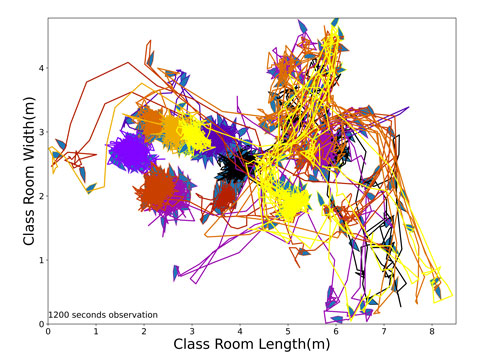
Emitted every quarter of a second, the signals bounced off sensors placed in the corners of each classroom, enabling the researchers to continuously measure not only how long and how close each child came to every other classmate and their teachers, but their precise physical orientation. Then, when COVID-19 closed schools last March, the researchers realized their novel data could enable them to simulate the spread of the highly contagious virus on a microscale not possible with the standard epidemiological models that usually quantify transmission on a societal level.
“No one else has such high-resolution data tracking the movement of kids, so when the pandemic started we asked, ‘How can we use our data to tackle COVID-19?’ ” said Chaoming Song, associate professor of physics and the senior author of the study, which is available on the open-access arXiv.org site for pre-print scientific papers.
“More importantly, our technology tracks and records the orientation of each child,” continued Song, an expert in the evolution of networks. “So, it’s not only about their locations but also about their angles, if they’re face to face or not. Standard models just approximate these details. Our model is very refined—about angles, about locations, about how every individual moves every quarter of a second.”
To simulate the spread of COVID-19 among preschoolers, who are not eligible for the coronavirus vaccination, the researchers combined their data on the interaction patterns of each of the 50 students and 11 teachers with a number of other variables, including transmission rates published by the Centers for Disease Control and Prevention. Then, to estimate the transmission impact of an infected but asymptomatic individual attending class, they ran thousands of simulations that, one by one, assumed each student or each teacher was patient zero—the first person who unwittingly brought COVID-19 into each of the four classrooms.
“The key thing about patient zero is that they’re asymptomatic when they go to school,” Messinger said. “Otherwise, we assumed that they wouldn’t go to school. That’s also an important message: If your kid is sick, do not send them to school.”
The researchers also calculated the impact of each patient zero on the proportion of overall infections, the average transmission rate, and the lag time before the first symptomatic individuals appeared under multiple scenarios, including the consequences of vaccinated teachers teaching classes at half capacity. That’s how they arrived at their conclusion that decreasing classroom density and ensuring teacher vaccinations would lead, respectively, to a 13.1 percent and a 12.5 percent drop in overall infections.
While the current model did not focus on the Delta variant of COVID-19, Song said, he believes lower class densities, which would enable greater social distancing, would likewise curtail the spread of the more virulent strain—especially with Miami-Dade’s mandatory mask mandate. He said the research team plans to work on a model that accounts for both masks and the Delta variant.
To develop their current model, Song, Messinger, and Perry worked with longtime collaborator Mei-Ling Shyu, professor and associate chair of the Department of Electrical and Computer Engineering, and also enlisted Prem R. Warde, the director of process improvement and data science who runs the University of Miami Health System’s COVID-19 predictive models.
While providing feedback on the design of the classroom model and many of its parameters, Warde gained the idea of using radio frequency tags to monitor the localized spread of COVID-19, or other pathogens, in the hospital setting.
“I actually didn’t even think about doing radio frequency identification analysis before I started talking with them,” said Warde, a member of the University of Miami Hospitals and Clinics’ Care Transformation team and Data Analytics Research Team. “Which is something we should consider because yes, you can report national numbers, you can report state levels, but in reality, the epidemic is localized to each individual community, and it’s important to be able to understand and respond to those fluctuations.”
In addition to Song, Messinger, Perry, Warde, and Shyu, other co-authors of the study include its two lead authors—Yi Zhang, one of Song’s graduate students, and Yudong Tao, one of Shyu’s graduate students.

